The first reports of a disease caused by the severe acute respiratory syndrome Coronavirus-2 was in Wuhan, China, in December 2019. The World Health Organisation (WHO) declared the outbreak a Public Health emergency of international concern on 30 January 2020 and a pandemic on 11 March 2020. Today, more than 100 million cases of COVID-19 have been reported in more than 188 countries, resulting in over 2 million deaths.
Most of the world was slow to respond and when they did many governments responded by implementing travel restrictions, lockdowns and facility closures. The pandemic and subsequent response has caused global social and economic disruption, including the largest global recession since the Great Depression and global famines affecting 265 million people. It has led to the postponement or cancellation of sporting, religious, political, and cultural events. Schools, universities, and colleges have also been closed either on a nationwide or local basis in 172 countries, affecting approximately 98% of the world’s student population.
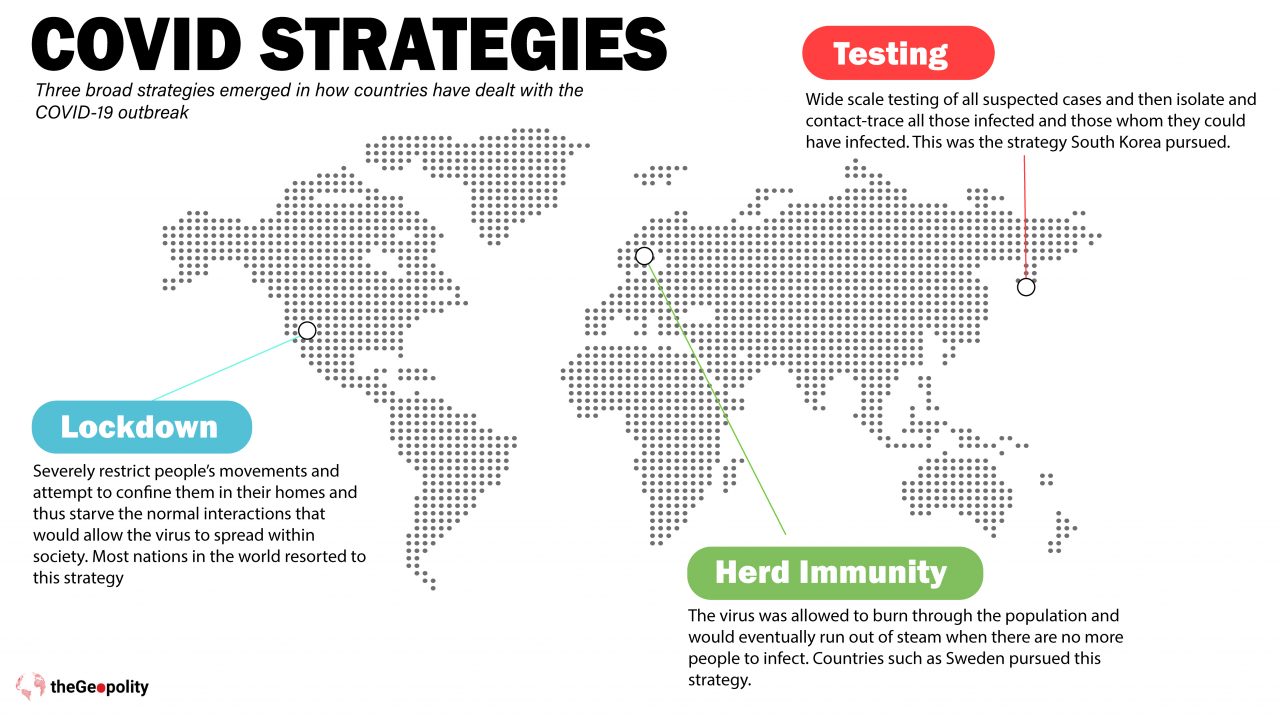
Three broad strategies emerged in how countries have dealt with the COVID-19 outbreak, the herd immunity approach, the lockdown method and testing. All three strategies had some rationale as well as trade-offs. The herd immunity approach may have helped build immunity in the long term and allow societies to continue to function (at least in the short term) but it posed a significant risk to vulnerable members of society. It could easily lead to mass infections and hospitalisations that lead to overwhelming the health services and thus greater mortality rates.
As for the lockdown method, this had massive implications on the economy and the lives of everyone within society. It can be effective, if one is to believe the figures that came out of China, but needed to be implemented very early and have to be total in its application. However, the long-term impact on people’s lives has been devastating. Loss of income and businesses and potential devastation to people’s lives (even some unintended deaths). Lockdowns took national economies offline and devastated jobs, GDP and investments. In many cases the lockdowns were far worse than the virus itself. The UK, US, Germany, Eurozone saw their economies shrink in excess of 10% in just one quarter. Whilst a recession was expected in 2020, such contractions are great depression territory. India and the US saw 25% of their workforce lose their jobs, whilst Russia, Canada and Austria saw job losses of over 10% for their workforce.
Governments across the world attempted to soften the blow by providing payroll support and grants, but such a large drop due to lockdowns affected markets, supply chains, investments and the future prospects of whole industries. The damage of lockdown to economies has been immense.
The wide scale testing of people has been implemented in places such as South Korea, Singapore and Japan: it has allowed normal day to day businesses and lives to continue for the vast majority of healthy people within society. Schools remained open, restaurants, shops and even places of worship. It’s been shown to have dramatically slowed the infection rates and even reversed them in some countries. It allows greater targeting of care for the vulnerable and thus better medical treatment and outcomes (and lower mortality rates). But the main prerequisite for this approach is that it requires good societal infrastructure. Countries like Singapore and South Korea developed these strategies due to their experiences with SARS and even MERS. It meant they were able to act fast, locate people who even shared taxi journeys with infected drivers as well as people who were at the same restaurants.
Most of the world pursued lockdown as a strategy and this has left significant damage to national economies and the global economy. The second round of lockdowns has made the situation created by the first lockdowns worse and will make recovery longer and more difficult for the global economy.
Most of the world pursued lockdown as a strategy and this has left significant damage to national economies and the global economy
Assessing China’s COVID Response
Just over a year ago, on 23 January 2020 the world witnessed the first organised lockdown due to the coronavirus. Wuhan in China became the most famous city in the world due to the virus reportedly beginning from there. On its first anniversary Wuhan celebrated its battle with COVID rather quietly. It is now remembered not as a disaster but as a victory, something the Communist Party has used to project its credibility around the world. In a report released in March 2020, the World Health Organisation (WHO) congratulated China on a “unique and unprecedented public health response [that] reversed the escalating cases.”[1] China has received much praise for her response to the COVID-19 pandemic as well as some severe criticism, but the Chinese Communist Party (CCP) has taken full credit for halting the spread of the virus.
The first confirmed patient who started experiencing symptoms was on 1 December 2019 in the Hubei province. The 57-year-old woman subsequently tested positive for COVID-19 and is likely patient zero in the coronavirus pandemic.
The outbreak went unnoticed until a cluster of unknown pneumonia cases were observed by Zhang Jixian, director of the Department of Respiratory Medicine at Hubei Hospital of Integrated Traditional Chinese and Western Medicine, whose experience fighting SARS in 2003 kept her alerted about a public health emergency. On 26 December 2019, a couple of senior citizens who lived near Zhang’s hospital came to her for their fever and cough. On the same day, a patient from Huanan Seafood Market that Dr. Zhang saw also had the unusual conditions. On 28 and 29 December, three more patients who had visited the Huanan Seafood Market visited the clinic of the hospital. The hospital notified the provincial and municipal health commissions.
Wuhan health authorities quickly investigated and, amid social media leaks, publicly announced details about the outbreak on 31st December 2020, closing the suspect market on 1st January 2020. National health authorities took control of the investigation and Chinese scientists rapidly identified a new coronavirus, preliminarily confirmed it as the cause of the atypical pneumonia, completely sequenced its genome in record time, developed testing kits, and published multiple sequences through globally-accessible databases on 11 January 2020.

Denial
Several doctors who came to be known as the whistle-blower doctors were warned by Wuhan’s police for ‘spreading misinformation’ and were summoned by the police on 3 January 2020. Dr Li Wenliang, one of the whistle-blowers died from the virus on 7 February 2020. By early June 2020, five more doctors from the whistle-blower hospital in Wuhan died from COVID-19. The death of Dr. Li led to widespread criticism of China’s regime. A subsequent Chinese official inquiry exonerated Dr. Li, and the CCP formally offered a ‘solemn apology’ to his family and revoked the admonishment of him.
The Chinese authorities did not immediately notify the WHO as required of its member states, although the WHO obtained information from other sources. Chinese authorities rebuffed requests for samples and offered to assist with epidemiological investigations from the WHO and the US government. Initially focused on a theory of animal-borne disease, they downplayed — though never denied — the possibility of highly-infectious human-to-human transmission. In updates during the outbreak’s first critical weeks, Wuhan officials advised residents to guard against seasonal infectious diseases by wearing masks, avoiding closed or crowded spaces and seeing a doctor if experiencing fever or respiratory symptoms, but did not highlight increased potential risk from the outbreak.
By the second week of January 2020 Wuhan city was overwhelmed with thousands of new cases of coronavirus each day. In mid-January 2020, the Chinese authorities introduced unprecedented measures to contain the virus, Wuhan was placed under a strict lockdown that lasted 76 days. Public transport was suspended. Soon afterwards, similar measures were implemented in every city in Hubei province. All movement in and out of Wuhan and 15 other cities in Hubei province — home to more than 60 million people — was halted. Flights and trains were suspended and roads were blocked. Soon after, people in many Chinese cities were told to stay at home and venture out only to get food or medical help. Some 760 million people, roughly half the country’s population, were confined to their homes.
Across China, 14,000 health checkpoints were established at public transport hubs. School reopenings after the winter vacation were delayed and dozens of cities implemented family outdoor restrictions, which typically meant that only one member of each household was permitted to leave the home every couple of days to collect necessary supplies. Within weeks, China had managed to test 9 million people for COVID-19 in Wuhan. It set up an effective national system of contact tracing. As the world’s largest manufacturer of personal protective equipment, it was relatively straightforward for China to ramp up production of clinical gowns and surgical masks.
Chinese authorities also built two dedicated hospitals in Wuhan in about 1 week, sent health care workers from all over China to Hubei, and launched an unprecedented effort to trace contacts of confirmed cases. In Wuhan alone, more than 1,800 teams traced tens of thousands of contacts. Aggressive ‘social distancing’ measures were also implemented in the entire country including cancelling sporting events and the closure of theatres, schools, and businesses.
Two widely used mobile phone apps, AliPay and WeChat—which in recent years have replaced cash in China— helped enforce the restrictions, because they allowed the government to keep track of people’s movements and even stop people with confirmed infections from travelling.
“As a consequence of all of these measures, public life is very reduced. But the measures did work. In the end, infected people rarely spread the virus to anyone except members of their own household. Once all the people living together were exposed, the virus had nowhere else to go and chains of transmission ended. That’s how the epidemic truly came under control.”[2] These were the observations in the WHO report released on 28 February 2020 by a team of 12 Chinese and 13 foreign scientists who toured five cities in China to study the state of the COVID-19 epidemic and the effectiveness of the country’s response. It was organised jointly by the WHO and the Chinese government. The report also found: “China is unique in that it has a political system that can gain public compliance with extreme measures. The country also has an extraordinary ability to do labour-intensive, large-scale projects quickly. No one else in the world really can do what China just did.”[3]
But critics say the report failed to acknowledge the costs of the most severe measures imposed by China’s regime: massive lockdowns and electronic surveillance of millions of people. “I think there are very good reasons for countries to hesitate using these kinds of extreme measures,” said Lawrence Gostin, a global health law scholar at Georgetown University.
Epidemiologists say China’s mammoth response had one glaring flaw: it started too late. In the initial weeks of the outbreak in December and January 2020, Wuhan authorities were slow to report cases of the mysterious infection, which delayed measures to contain it, said Howard Markel, a public-health researcher at the University of Michigan in Ann Arbor. “The delay of China’s action is probably responsible for this world event,” said Markel.
China managed to get a grip on the spread of COVID-19 by isolating the regions where the disease outbreak started, after an initial period of suppression of the information.[4] Reports show that officials in China hid evidence of a serious infectious disease from as early as mid-December 2019. By 3rd January 2020, China had 44 patients with a mysterious disease. The new virus was finally acknowledged on 7th January 2020. However, the city of Wuhan was not placed under a lockdown until 23rd January 2020 – and international flights were only restricted even later. So, the policy might have helped China but did not stop the spread globally. By mid-January 2020, there were cases across South East Asia, but even those countries were not advised by the WHO to restrict travel.
Epidemiologists say China’s mammoth response had one glaring flaw: it started too late. In the initial weeks of the outbreak in December and January 2020, Wuhan authorities were slow to report cases of the mysterious infection, which delayed measures to contain it
When the world first started learning about the outbreak of the new respiratory virus in the city of Wuhan, the Chinese government was defensive and secretive about it. Many foreign commentators were quick to cast China’s reaction as a metaphor for the inherent weaknesses of an authoritarian system. Although it came at the cost of intense restrictions, people in Wuhan, China squeezed the life out of the virus and out of its ability to spread. Then, just as COVID-19 began to fade in China, the pandemic took off in Europe—first in Italy and then throughout the continent.
Sweden’s Herd Strategy
Sweden has been credited for not having a draconian lockdown as it pursued herd immunity for her 10 million population. Sweden avoided a lockdown and instead emphasised personal responsibility, social distancing and good hygiene in a bid to slow rather than eradicate the disease. By eschewing lockdown and aiming for herd immunity Sweden may now be paying a heavy price.
Swedish public health authorities have defended their decision not to lock down the country in response to the global COVID-19 pandemic in March 2020. Schools were closed to children over 16 and gatherings of more than 50 people were discouraged, but bars, restaurants, and other public spaces remained open, and citizens were trusted to distance themselves. At the heart of the government’s strategy was the implicit idea that, rather than contain the spread of the disease, a country could achieve herd immunity by allowing a proportion of the population to be infected—at the expense of deaths among the vulnerable. As case numbers drastically increased around the world and death tolls rose across Europe, Swedish experts, and indeed the public, remained supportive of the strategy.
In spring, at a time when countries across Europe were recording alarming surges in daily COVID-19 infections, Sweden had recorded her lowest rate of positive tests since the virus emerged, leading many to question whether the Nordic country’s relaxed approach to lockdown paid off. The small country of 10 million people carried out a record number of new coronavirus tests in November 2020, with the national health agency reporting that only 1.2% coming back positive, the lowest rate since the pandemic began and much better than many countries on the continent.
Sweden has had one of the highest death rates per total population in Europe with this strategy. More than half the deaths occurred in care homes for older people. Anders Tegnell, who led the strategy as the state epidemiologist admitted too many have died.[5] Sweden’s higher rates of viral infection, hospitalisation and mortality compared with neighbouring countries raises many questions about pursuing herd immunity as a strategy. The strategy may have serious implications for Scandinavia and beyond. In May 2020, the WHO said that global studies had found antibodies in only 1-10% of the global population, with similar findings emerging from Spain and France. The agency warned against any country depending on herd immunity as a strategy. Sweden failed to protect her elderly population, who made up the majority of those who died from COVID-19 there.
This speaks to the difficulty of applying an idealistic, laboratory model of separating the infected from the most vulnerable to the real world: The country reported her highest death tally in 150 years in the first half of 2020. Despite these efforts, it’s a relatively small size compared to the UK and the US, Sweden is not even close to achieving herd immunity.
One the first anniversary of the pandemic the nations in the Far East are seen to have dealt effectively with the virus, whilst the western countries who have established healthcare systems have struggled to deal with the virus. This is why confidence in political leaders in the west is at all-time lows. Many populist leaders have attempted to deflect attention by resorting to conspiracies and blaming others. As vaccines are manufactured, distribution and healthcare nationalism is already growing and will impact the response to the virus.
[1] Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19), https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
[2] Ibid
[3] Ibid
[4] Blocking information on COVID-19 can fuel the spread of misinformation, Nature, 30 March 2020, https://www.nature.com/articles/d41586-020-00920-w
[5] Coronavirus: Sweden’s Tegnell admits too many died, BBC online, 3 June 2020, https://www.bbc.co.uk/news/world-europe-52903717